Diagnosis of Obstructive Sleep Apnea
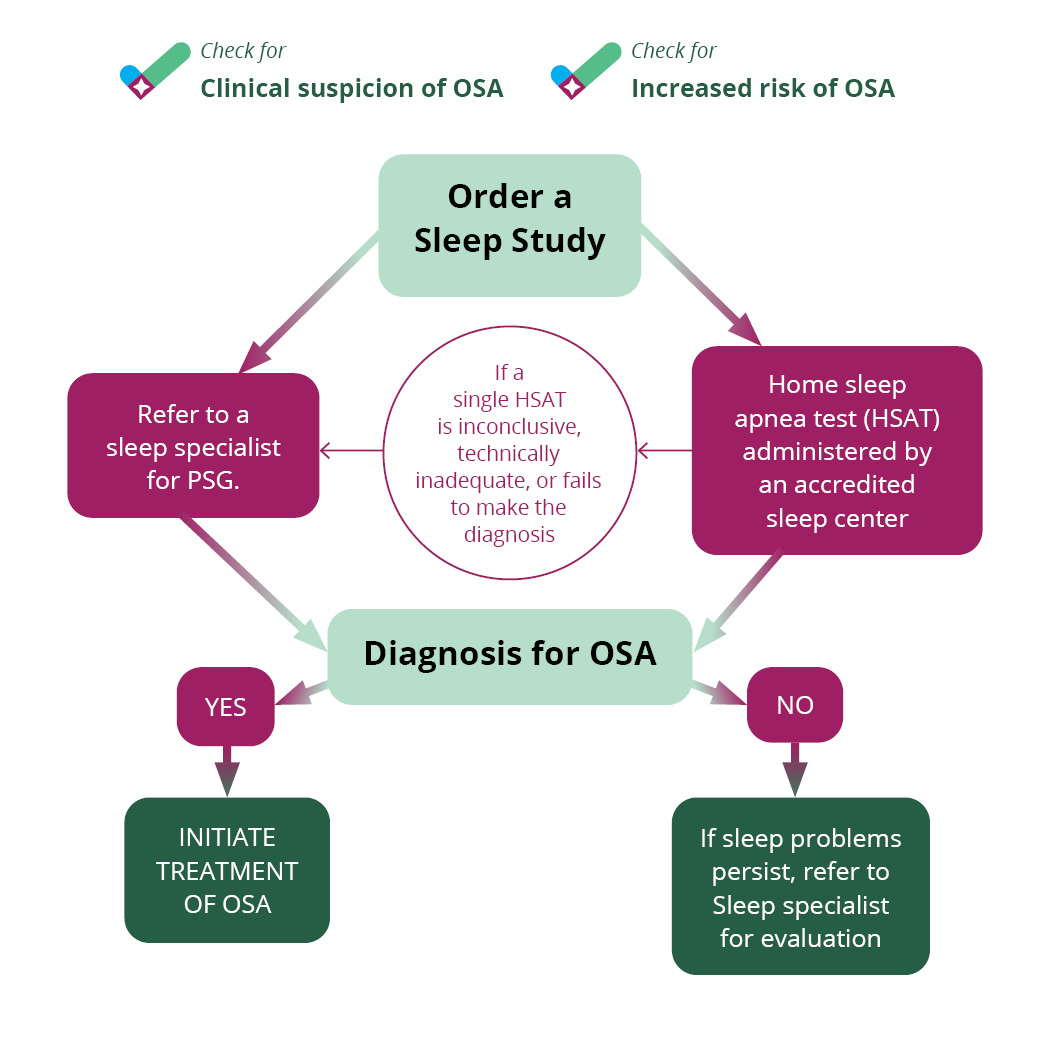
If the patient evaluation provides clinical suspicion of obstructive sleep apnea, a primary care provider can order a sleep study or refer the patient to sleep physician for further evaluation. Treatment of OSA will improve patients’ sleep, overall health and quality of life, and reduce the risk of complications from comorbidities.
Clinical suspicion of OSA
Wake Symptoms
- Daytime sleepiness – falling asleep inappropriately (at driving, work, school, meetings, conversations, other sedentary activities
- Morning headaches
- Mood changes
- Forgetfulness
- Difficulty with focus or concentration
- Car crashes (especially single-vehicle, rear-ending another vehicle, off-road deviation)
- Declining work performance
- Absenteeism (school, work)
- Presenteeism (school, work) – in attendance, but not performing your best
Sleep Symptoms*
- Loud, habitual snoring (can be disruptive to others)
- Choking/gasping
- Others say you stop breathing during sleep
- Fragmented sleep, insomnia
- Unrefreshing sleep
- Frequent urination at night
- Nightmares
* most patients are unaware they have sleep apnea; more than 85% of cases remain undiagnosed
Increased risk of OSA
- Obesity (BMI > 35)
- Congestive heart failure
- Atrial fibrillation
- Treatment refractory hypertension
- Type 2 diabetes
- Nocturnal dysrhythmia
- Stroke
- Pulmonary hypertension
- High-risk driving populations
What is a sleep study?
There are two common types of sleep studies: in-lab polysomnography (PSG) and home sleep apnea test (HSAT). An overnight in-lab PSG administered by an accredited sleep center is considered the gold standard sleep study. It provides the most comprehensive evaluation of a patient’s sleep, recording brain waves, heart rate and breathing.
Home sleep apnea testing may be recommended in patients with a high likelihood of moderate to severe sleep apnea or those with no significant medical conditions related to sleep apnea. HSATs contain sensors to collect breathing and blood oxygen levels during sleep. Patients can set up the testing equipment themselves.
Both PSGs and HSATs should be read and interpreted by a sleep specialist for an accurate diagnosis. Sometimes, an HSAT records incomplete data, and a follow-up PSG may be necessary.
If the patient is diagnosed with sleep apnea, they should be referred to a sleep specialist to discuss treatment options (link to treatment algorithm page). If the patient is not diagnosed with sleep apnea but continues to have sleep problems, referral to a sleep specialist is advised to evaluate for other sleep disorders. About 70 million people experience sleep disorders every year.
OSA is a serious but common health condition that can be treated and managed. Treating OSA can improve a patient’s health and quality of life, decreasing the chance of serious health problems, motor vehicle accidents, daytime sleepiness, irritability and difficulty concentrating.
