Screening for Obstructive Sleep Apnea
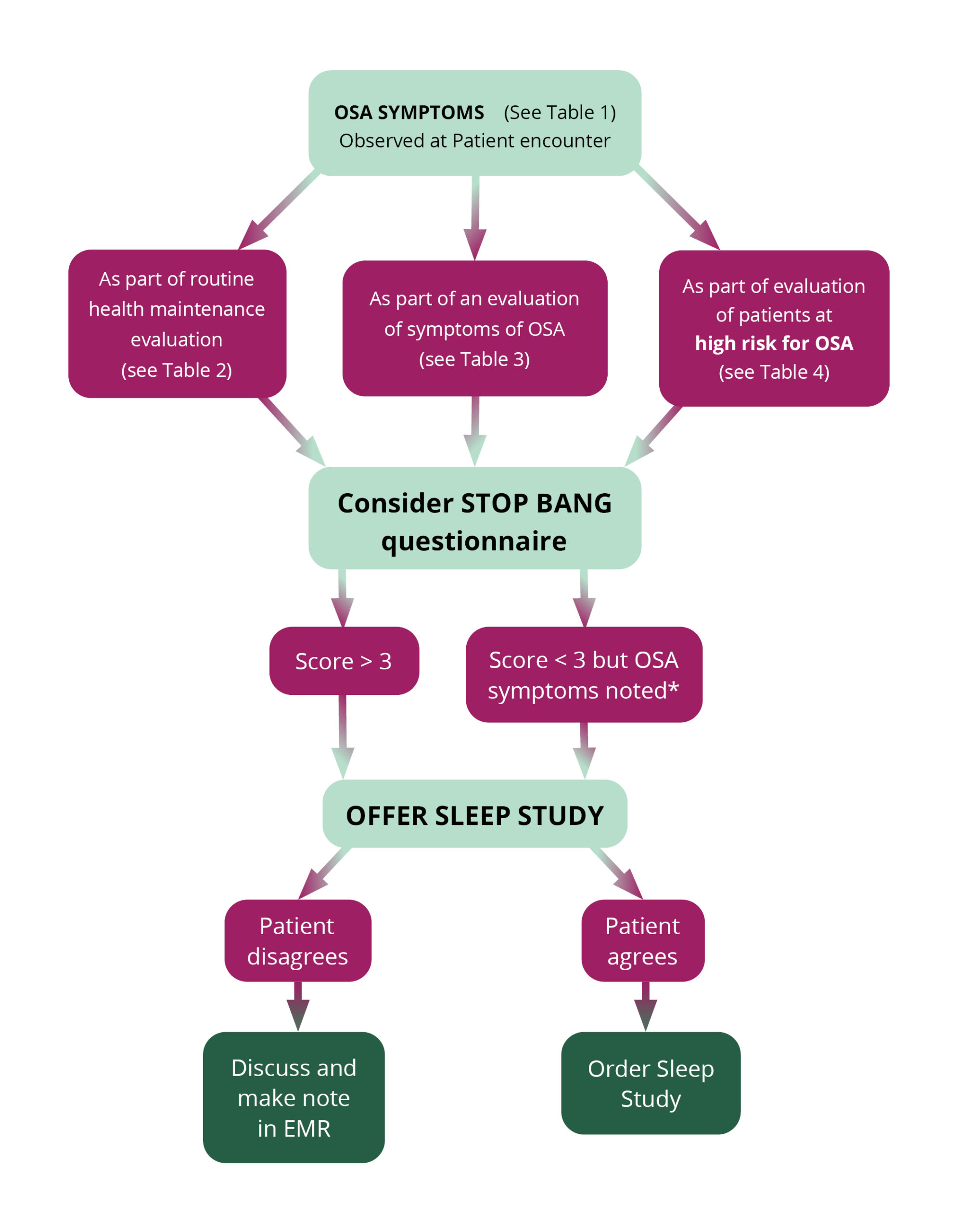
Patients who exhibit symptoms or risk factors of obstructive sleep apnea (OSA) should be screened to determine if they may have OSA prior to testing for the disorder. The algorithm below provides a detailed procedure for use by healthcare professionals in their practice which illustrates how patients should be screened for OSA.
A downloadable version and additional information and screening resources are available following the algorithm.
| Table 1 – Symptoms of OSA | |
|---|---|
| Wake Symptoms | Sleep Symptoms* |
| Daytime sleepiness – falling asleep inappropriately (at driving, work, school, meetings, conversations, other sedentary activities) | Loud, habitual snoring (can be disruptive to others) |
| Morning headaches | Choking/gasping |
| Mood changes | Others say you stop breathing during sleep |
| Forgetfulness | Fragmented sleep, insomnia |
| Difficulty with focus or concentration | Unrefreshing sleep |
| Car crashes (especially single-vehicle, rear-ending another vehicle, off-road deviation) | Frequent urination at night |
| Declining work performance | Nightmares |
| Absenteeism (school, work) | |
| Presenteeism (school, work) – in attendance, but not performing your best | |
| Table 2 – Questions about OSA that Should Be Included in Routine Health Maintenance Evaluations | |
|---|---|
| Is the patient obese? | |
| Is the patient retrognathic? | |
| Does the patient complain of daytime sleepiness? | |
| Does the patient snore? | |
| Does the patient have hypertension? |
| Table 3 – OSA Symptoms That Should Be Evaluated During a Comprehensive Sleep Evaluation | |
|---|---|
| Witnessed apneas | |
| Snoring | |
| Gasping/choking at night | |
| Excessive sleepiness not explained by other factors | |
| Non-refreshing sleep | |
| Total sleep amount | |
| Sleep fragmentation/maintenance insomnia | |
| Nocturia | |
| Morning headaches | |
| Decreased concentration | |
| Memory loss | |
| Decreased libido | |
| Table 4 – Patients at High Risk for Sleep Disordered Breathing (including OSA) | |
|---|---|
| Obesity (BMI > 35) | |
| Congestive heart failure | |
| Atrial fibrillation | |
| Treatment refractory hypertension | |
| Type 2 diabetes | |
| Nocturnal dysrhythmias | |
| Stroke | |
| Pulmonary hypertension | |
| High-risk driving populations | |
| Decreased concentration | |
What is a sleep study?
A sleep study is a non-invasive, overnight exam that is used to diagnose sleep disorders. The test measures specific sleep characteristics and parameters to determine if a patient has sleep disorders such as sleep apnea, periodic limb movement disorder, narcolepsy, restless legs syndrome, insomnia, and REM sleep behavior disorder. There are two types of sleep studies: polysomnography or in-lab (PSG) and home sleep apnea test (HSAT).
A medical provider or a sleep doctor may recommend a sleep study to:
- Test for sleep-related breathing disorders including sleep apnea
- Evaluate abnormal behaviors during sleep due to parasomnias
- As part of the evaluation of narcolepsy or other hypersomnia-related disorders
- Adjust the levels of airflow in patients who receive CPAP therapy for sleep-related breathing disorders (CPAP titration)
- Determine why treatment for a sleep disorder is not working
What is a polysomnography (PSG) sleep study?
PSG is a test that provides comprehensive evaluation of a patients’ sleep. The patient is required to stay overnight at a sleep center or a hospital where a sleep technician monitors them and oversees the test. A variety of functions such as heart rate, breathing, eye movement, brain activity, muscle tone, respiratory effort, airflow, snoring, blood oxygen levels, body position, etc., are measured and recorded throughout the night. It also tracks the patient’s arm and leg movements.
What is a split night study?
A split night sleep study combines diagnostic evaluation for a minimum of two hours followed by PAP (positive airway pressure) titration during the remaining portion of the procedure. Ideally a minimum of three hours of PAP evaluation is required.
Most patients do not qualify for a split night sleep study, but the American Academy of Sleep Medicine recommends its implementation when during the first two hours of diagnostic evaluation of the study there is:
- AHI of ≥ 40 events/hour of sleep, or
- AHI of ≥ 20 and < 40 events/per hour of sleep and there is the evidence of cardiac arrhythmias or significant and persistent oxyhemoglobin desaturation
What is a home sleep apnea test (HSAT)?
Some patients with a high probability for having sleep apnea and no other medical disorders may be candidates for a home sleep apnea test. This type of sleep study lets you sleep in your own home while a small monitor collects data as you sleep. The testing equipment is less complicated than what is used in an in-lab sleep study. After home sleep apnea test, the device is taken back to medical provider or sent in by mail.
There are different types of HSAT which can change over time. The type of devices available today include flow-based, tonometry-based, or other types.
A follow up should be scheduled after the test to decide best treatment or make the appropriate referral.